How Does Narcan Work: The Secret Life of a “Miracle Drug”
Article Contents
Narcan can—literally—raise the dead. Both those who have suffered an opioid overdose, as well as the first responders who resuscitated them, can agree on one thing; Narcan, or naloxone, is fast and effective at reversing the effects of opioid drugs.2
It only takes minutes for an opioid overdose to cause potentially fatal consequences. So it’s no surprise that many emergency personnel who have administered Narcan praise the fast-acting drug as nothing short of miraculous.
However, the people being rescued may describe the experience as “jarring” and even “painful.” This may seem contradictory but, with a better understanding of what this drug is and how it works, both reactions make sense and provide insight into the nature of—and treatment for— opioid addiction.
What is Narcan (Naloxone)?
Narcan is one brand name of the prescription drug naloxone. It is used to rapidly reverse the effects of an overdose from opioid drugs. Narcan, specifically, is now sold as a nasal spray form of naloxone or most commonly injected intramuscularly.1 Opioid drugs include heroin as well as prescription pain medications such as morphine, codeine, and oxycodone.
How Does Naloxone Work?
Signs of recovery are typically observed within 30 seconds to 2 minutes after administration, with repeat dosing sometimes being indicated. The victim’s breathing rate will increase, offsetting the most obvious imminent threat during an overdose; severe respiratory depression. There is also an associated increase in heart rate, cardiac output, and arterial blood pressure.6 Opioids depress the central nervous system so much that the victim can actually “forget to breathe.” This cuts oxygen off to the brain, which can result in brain damage or death if not reversed immediately. Therefore, Narcan becomes critically important with reversing this respiratory depression.
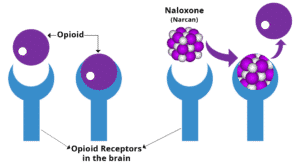
As heart rate and breathing begin to stabilize, the user regains consciousness and will appear responsive. Upon waking, however, euphoric feelings associated with an opioid high will be noticeably absent in the victim. This is because Narcan works as a “competitive opioid antagonist”; it competes with—and quickly overcomes—an opioid’s ability to bind to cellular receptors.2 These receptors function like biochemical gatekeepers and control various biological processes. Opioid molecules have a unique shape and configuration that specifically attach to opioid receptors, consequently activating whatever biological process that receptor regulates.
This, in turn, activates a process in the brain that activates the pleasure center in the brain. Non-drug users may activate this center when, for example, eating delicious food. Opioid receptors control this “reward mechanism” in the brain that uses pleasurable feelings as a “bribe” for completing basic life functions.3 After all, you have to eat to survive. Activating opioid receptors also aids in the relief of pain, and so opioids are often prescribed after injuries or operations.
However, when the mu opioid receptors are repeatedly activated by exogenous ingestion/intake of opioids, a “conditioned association” to the drug develops. This makes repeated usage likely in order to attain that pleasurable sensation. Each subsequent exposure further reinforces this conditioning, often leading to habitual drug use.3 The user then plunges into a downward spiral of escalating dose and duration of use.
Tolerance to the drug increases along with the user’s dependence on it. Addiction becomes all but inevitable as the user’s brain function inverts; to feel “normal” requires opioids in the user’s system. In fact, long-time users feel so abnormal when not on drugs that avoiding withdrawal symptoms becomes one of—if not the most—powerful driving forces with regards to their addition.5 Tragically, this makes the risk of an overdose, not a question of if, but . It’s at this fatal point that Narcan is often used to swiftly intervene.
Narcan works almost instantaneously because it disrupts the contact point between the opioid molecule and mu opioid receptor.
No matter how much of the drug is circulating in the user’s system, potency always depends on the availability of the mu opioid receptors. Thus, if the receptor is sufficiently blocked or occupied, the opioid is rendered useless.2
Think about it as being similar to a fingerprint scanner built into an iPhone. The phone will only unlock when the fingerprint it’s programmed to recognize makes contact with the scanner. If you were to stick a thick, black strip of masking tape over the scanner, the phone will become impossible to unlock. Antagonist drugs like Narcan “block” cell receptors in the same way. Better yet, while Narcan certainly binds to the receptor, it doesn’t activate it or “unlock” the process that produces a high. Narcan simply knocks the opioid molecule off the receptor, takes its place, and blocks further access.2
As a result of rapid redistribution throughout the body, naloxone has a very short duration of action; approximately 30-45 minutes.7 This is why another dose of Narcan is sometimes necessary for preventing re-occurrence of overdose symptoms. This is especially relevant in cases of extremely high dosages or opioids with a prolonged half-life, as the user will again be at risk once Narcan wears off2.
Broader challenges also come to light when treating long-term opioid addicts with Narcan. While these are often the users most at risk of overdosing, these are the most vulnerable to the deliberating after-effects felt when abruptly “coming down” from an opioid high. Put simply, they are at risk of experiencing severe withdrawal symptoms2. Ironically, Narcan’s miraculous ability to quickly avert the crisis of an overdose is also why so many users say they’re left intensely craving the same drug that almost took their life. If users are kept trapped in this cycle of addition, Narcan is only a temporary “Band-Aid” solution. Of note, the FDA has even approved Naltrexone skin implants to avoid overdoses.4
Opioid addition should be treated with the same life-and-death severity as the overdose or else Narcan is giving addicts another chance to live without another chance at life.6
References
- ADAPT Pharma. (2018). Narcan Nasal Spray 4mg. Retrieved 30 March, 2019 from https://www.narcan.com
- Jauncey, M. E., & Nielsen, S. (2017). Community use of naloxone for opioid overdose. Australian Prescriber, 40(4), 137-140.
- Le Merrer, J., Becker, J. A., Befort, K., & Kieffer, B. L. (2009). Reward processing by the opioid system in the brain. Physiological Reviews, 89(4), 1379–1412. doi:10.1152/physrev.00005.2009
- McGinley, L. (2016). FDA approves new way to treat opioid addiction – under the skin. Retrieved 30 March, 2019 from https://www.washingtonpost.com/news/to-your-health/wp/2016/05/26/new-implant-for-opioid-addiction-faces-likely-fda-verdict-friday/?utm_term=.213afb865711
- Morgan, M. M., & Christie, M. J. (2011). Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human. British Journal of Pharmacology, 164(4), 1322–1334. doi:10.1111/j.1476-5381.2011.01335.x
- Rzasa Lynn, R., & Galinkin, J. L. (2017). Naloxone dosage for opioid reversal: current evidence and clinical implications. Therapeutic Advances in Drug Safety, 9(1), 63–88. doi:10.1177/2042098617744161
- ScienceDirect. (2019). Naloxone – an overview. Retrieved 30 March, 2019 from https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/naloxone